By: Lori K. Madden, Venkatakrishna Rajajee, Theresa Human, Mark S. Wainwright, Mary Guanci, Shraddha Mainali, Shaun Rowe, Diane McLaughlin, John Lunde, Abhijit Lele & Herb Fried
Online First: 02 November 2021
Introduction
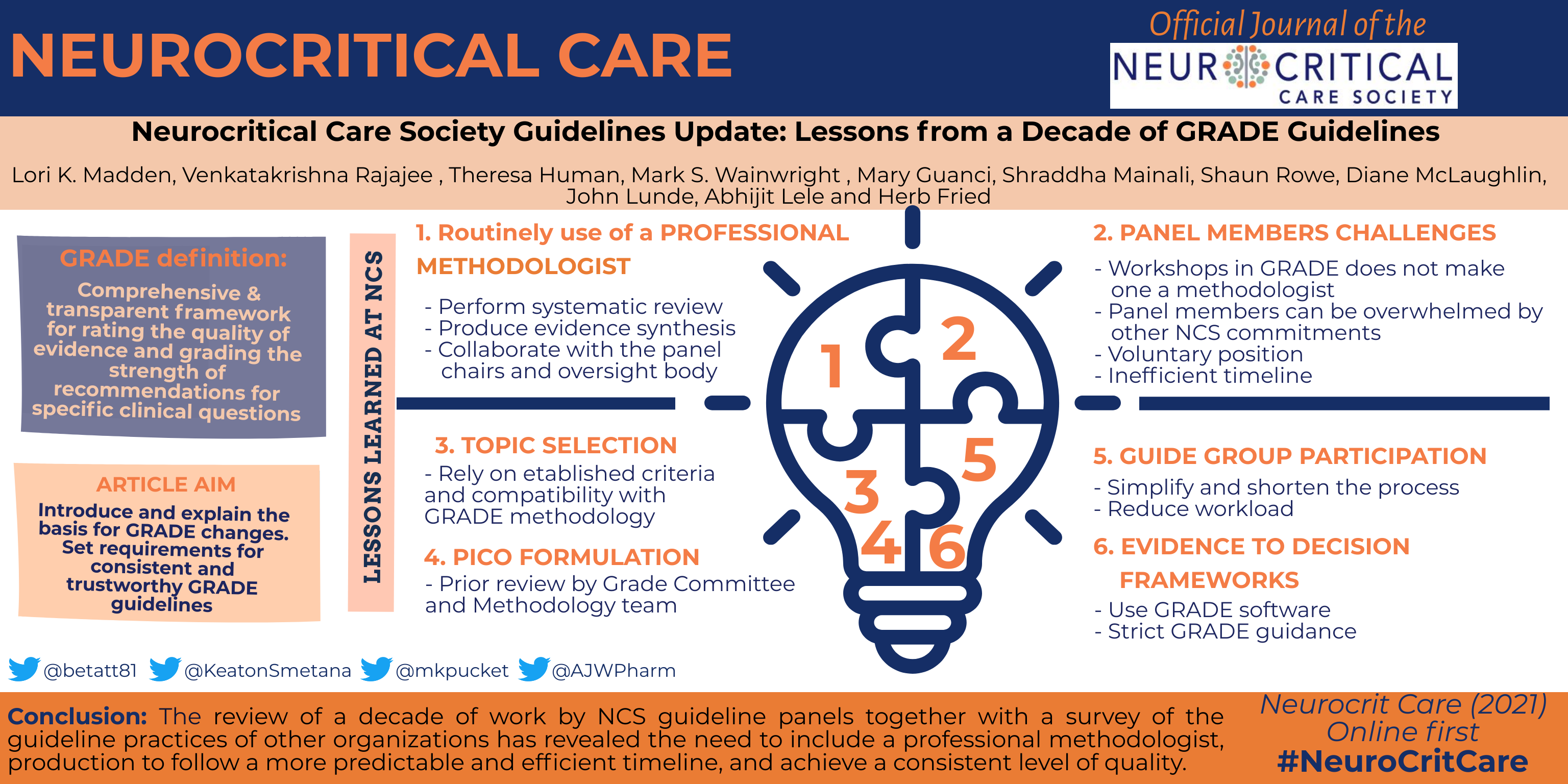
The Neurocritical Care Society (NCS) launched its clinical practice guideline program in 2012 with the publication of “Guidelines for the Evaluation and Management of Status Epilepticus” [1]. Work on this guideline coincided with the development of standards for trustworthy clinical practice guidelines by the Institute of Medicine (now the National Academy of Medicine) in 2011 [2]. These standards highlighted the need for rigorous and consistent evidence-based methodology aimed at producing clear, actionable recommendations relevant to the individual patient encounter. The NCS Guideline Committee (GC) made the prescient decision to adopt and implement an emerging methodology, Grading of Recommendations Assessment, Development and Evaluation (GRADE) [3], which has since been adopted or endorsed by more than 100 organizations worldwide. In the past decade, the US GRADE Working Group has elaborated, refined, and extended this methodology in many publications.
With the emergence of multiple GRADE-based guidelines since standards were developed, concerns were also raised about lack of adherence to published GRADE criteria in the development of these guidelines. In 2020, the US GRADE Working Group critically reviewed GRADE guidelines published in the National Guideline Clearinghouse [4]. Of the guidelines studied in this sample, which included two from NCS, nearly half did not comply with one or more of the key GRADE criteria for appropriate application of the methodology. Most commonly lacking were GRADE evidence profiles and evidence summaries, as well as explicit consideration of all four central domains required to move from evidence to recommendation. Those domains include certainty of evidence, balance of benefits to harms, patients’ values and preferences, and resource use and equity.
Read the full article